Introduction
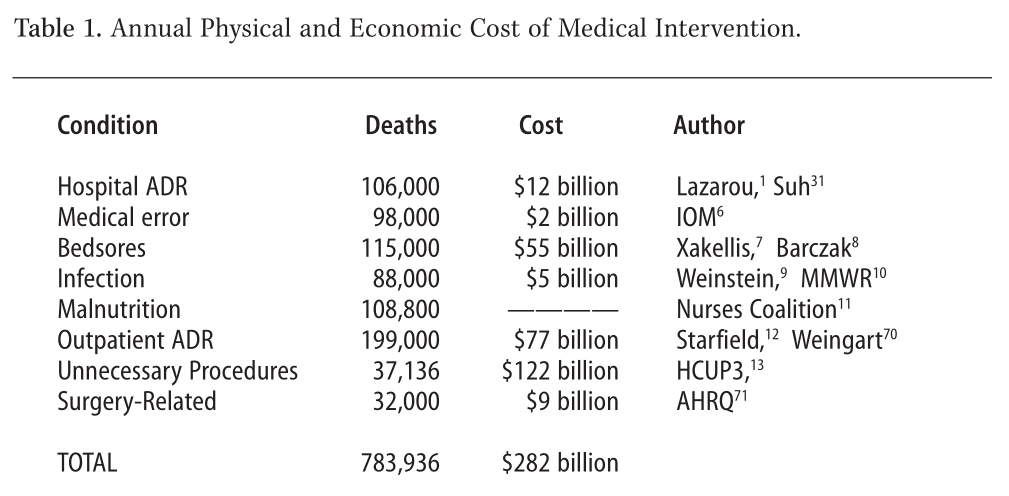
A close reading of medical peer-review journals and government health statistics shows that American medicine frequently causes more harm than good. The number of people having in-hospital, adverse drug reactions (ADR) to prescribed medicine is 2.2 million.1 Dr. Richard Besser, of the CDC, in 1995, said the number of unnecessary antibiotics prescribed annually for viral infections was 20 million. Dr. Besser, in 2003, refers to tens of millions of unnecessary antibiotics.2 The number of unnecessary medical and surgical procedures performed annually is 7.5 million.3 The number of people exposed to unnecessary hospitalization annually is 8.9 million.4 The total number of iatrogenic deaths shown in the Table 1, p.2 is 783,936.
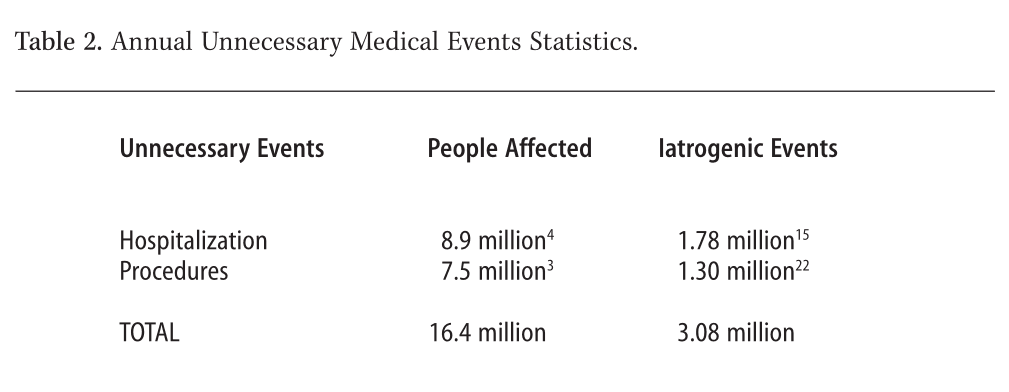
It is evident that the American medical system is the leading cause of death and injury in the United States. The 2001 heart disease annual death rate is 699,697; the annual cancer death rate, 553,251.5 The enumerating of unnecessary medical events is very important in our analysis. Any medical procedure that is invasive and not necessary must be considered as part of the larger iatrogenic picture. Unfortunately, cause and effect go unmonitored. The figures on unnecessary events represent people (“patients”) who are thrust into a dangerous healthcare system. They are helpless victims. Each one of these 16.4 million lives is being affected in a way that could have a fatal consequence. Simply entering a hospital could result in the following (see Table 2, p. 22):
- In 16.4 million people, 2.1% chance of a serious adverse drug reaction.1 (186,000)
- In 16.4 million people, 5-6% chance of acquiring a nosocomial infection.9 (489,500)
- In 16.4 million people, 4-36% chance of having an iatrogenic injury in hospital (medical error and adverse drug reactions).15 (1.78 million)
- In 16.4 million people, 17% chance of a procedure error.22 (1.3 million)
Overlap of Statistics
We have added, cumulatively, figures from 13 references of annual iatrogenic deaths. However, there is invariably some degree of overlap and double counting that can occur in gathering non-finite statistics. Death numbers don’t come with names and birth dates to prevent duplication. On the other hand, there are many missing statistics. As we will show, only about 5% to 20% of iatrogenic incidents are even recorded,15,17,18 and, our outpatient iatrogenic statistics12,55 only include drug-related events and not surgical cases, diagnostic errors, or therapeutic mishaps. We have also been conservative in our inclusion of statistics that were not reported in peer review journals or by government institutions. For example, on July 23, 2002, The Chicago Tribune analyzed records from patient databases, court cases, 5,810 hospitals, as well as 75 federal and state agencies and found 103,000 cases of death due to hospital infections, 75% of which were preventable.68 We do not include this figure but report the lower Weinstein figure of 88,000.9 Another figure that we withheld, for lack of proper peer review was The National Committee for Quality Assurance, September, 2003 report which found that at least 57,000 people die annually from lack of proper care for commons diseases such as high blood pressure, diabetes, or heart disease.69 Overlapping of statistics presented here may occur with the Institute of Medicine (IOM) paper that designates “medical error” as including drugs, surgery, and unnecessary procedures.6 Since we have also included other statistics on adverse drug reactions, surgery and, unnecessary procedures, perhaps a much as 50% of the IOM number could be redundant. However, even taking away half the 98,000 IOM number still leaves us with iatrogenic events as the number one killer at 734,936 annual deaths. Even greater numbers of iatrogenic deaths will eventually come to light when all facets of health care delivery are measured. Most iatrogenic statistics are derived from hospital-based studies. However, health care is no longer typically relegated to hospitals. Today, health care is shared by hospitals, outpatient clinics, transitional care, long-term care, rehabilitative care, home care, and private practitioners offices. In the current climate of reducing healthcare costs, the number of hospitals and the length of patient stays are being slashed. These measures will increase the number of patients shunted into outpatient, home care, and long-term care and the iatrogenic morbidity and mortality will also increase.
The First Major Iatrogenic Study
Dr. Lucien L. Leape opened medicine’s Pandora’s box in his 1994 JAMA paper, “Error in Medicine.”15 He began the paper by reminiscing about Florence Nightingale’s maxim – “first do no harm,” but he found evidence of the opposite happening in medicine. He found that Schimmel reported in 1964 that 20% of hospital patients suffered iatrogenic injury, with a 20% fatality rate. Steel in 1981 reported that 36% of hospitalized patients experienced iatrogenesis with a 25% fatality rate and adverse drug reactions were involved in 50% of the injuries. Bedell in 1991 reported that 64% of acute heart attacks in one hospital were preventable and were mostly due to adverse drug reactions. However, Leape focused on his and Brennan’s “Harvard Medical Practice Study” published in 1991.15a They found that in 1984, in New York State, there was a 4% iatrogenic injury rate for patients with a 14% fatality rate. From the 98,609 patients injured and the 14% fatality rate, he estimated that in the whole of the U.S. 180,000 people die each year, partly as a result of iatrogenic injury. Leape compared these deaths to the equivalent of three jumbo jet crashes every two days.
Why Leape chose to use the much lower figure of 4% injury for his analysis remains in question. Perhaps he wanted to tread lightly. If Leape had, instead, calculated the average rate among the three studies he cites (36%, 20%, and 4%), he would have come up with a 20% medical error rate. The number of fatalities that he could have presented, using an average rate of injury and his 14% fatality, is an annual 1,189,576 iatrogenic deaths, or over ten jumbo jets crashing every day. Leape acknowledged that the literature on medical error is sparse and we are only seeing the tip of the iceberg. He said that when errors are specifically sought out, reported rates are “distressingly high”. He cited several autopsy studies with rates as high as 35-40% of missed diagnoses causing death. He also commented that an intensive care unit reported an average of 1.7 errors per day per patient, and 29% of those errors were potentially serious or fatal. We wonder: what is the effect on someone who daily gets the wrong medication, the wrong dose, the wrong procedure; how do we measure the accumulated burden of injury; and when the patient finally succumbs after the tenth error that week, what is entered on the death certificate? Leape calculated the rate of error in the intensive care unit. First, he found that each patient had an average of 178 “activities” (staff/procedure/medical interactions) a day, of which 1.7 were errors, which means a 1% failure rate. To some this may not seem like much, but putting this into perspective, Leape cited industry standards where in aviation a 0.1% failure rate would mean 2 unsafe plane landings per day at O’Hare airport; in the U.S. Mail, 16,000 pieces of lost mail every hour; or in banking, 32,000 bank checks deducted from the wrong bank account every hour. Analyzing why there is so much medical error Leape acknowledged the lack of reporting. Unlike a jumbo jet crash, which gets instant media coverage, hospital errors are spread out over the country in thousands of different locations. They are also perceived as isolated and unusual events. However, the most important reason that medical error is unrecognized and growing, according to Leape, was, and still is, that doctors and nurses are unequipped to deal with human error, due to the culture of medical training and practice. Doctors are taught that mistakes are unacceptable. Medical mistakes are therefore viewed as a failure of character and any error equals negligence. We can see how a great deal of sweeping under the rug takes place since nobody is taught what to do when medical error does occur. Leape cited McIntyre and Popper who said the “infallibility model” of medicine leads to intellectual dishonesty with a need to cover up mistakes rather than admit them. There are no Grand Rounds on medical errors, no sharing of failures among doctors and no one to support them emotionally when their error harms a patient. Leape hoped his paper would encourage medicine “to fundamentally change the way they think about errors and why they occur.” It’s been almost a decade since this groundbreaking work, but the mistakes continue to soar. One year later, in 1995, a report in JAMA said that, “Over a million patients are injured in U.S. hospitals each year, and approximately 280,000 die annually as a result of these injuries. Therefore, the iatrogenic death rate dwarfs the annual automobile accident mortality rate of 45,000 and accounts for more deaths than all other accidents combined.”16 At a press conference in 1997, Dr. Leape released a nationwide poll on patient iatrogenesis conducted by the National Patient Safety Foundation (NPSF), which is sponsored by the American Medical Association. The survey found that more than 100 million Americans have been impacted directly and indirectly by a medical mistake. Forty-two percent were directly affected and a total of 84% personally knew of someone who had experienced a medical mistake.14 Dr. Leape is a founding member of the NPSF. Dr. Leape at this press conference also updated his 1994 statistics saying that medical errors in inpatient hospital settings nationwide, as of 1997, could be as high as three million and could cost as much as $200 billion. Leape used a 14% fatality rate to determine a medical error death rate of 180,000 in 1994.15 In 1997, using Leape’s base number of three million errors, the annual deaths could be as much as 420,000 for inpatients alone. This does not include nursing home deaths, or people in the outpatient community dying of drug side effects or as the result of medical procedures.
Only a Fraction of Medical Errors are Reported
Leape, in 1994, said that he was well aware that medical errors were not being reported.15 According to a study in two obstetrical units in the U.K., only about one quarter of the adverse incidents on the units are ever reported for reasons of protecting staff or preserving reputations, or fear of reprisals, including law suits.17 An analysis by Wald and Shojania found that only 1.5% of all adverse events result in an incident report, and only 6% of adverse drug events are identified properly.18 The authors learned that the American College of Surgeons gives a very broad guess that surgical incident reports routinely capture only 5-30% of adverse events. In one surgical study only 20% of surgical complications resulted in discussion at Morbidity and Mortality Rounds.18 From these studies it appears that all the statistics gathered may be substantially underestimating the number of adverse drug and medical therapy incidents. It also underscores the fact that our mortality statistics are conservative figures.
Drug Iatrogenesis
Drugs comprise the major treatment modality of scientific medicine. With the discovery of the “Germ Theory” medical scientists convinced the public that infectious organisms were the cause of illness. Finding the “cure” for these infections proved much harder than anyone imagined. From the beginning, chemical drugs promised much more than they delivered. But far beyond not working, the drugs also caused incalculable side effects. The drugs themselves, even when properly prescribed, have side effects that can be fatal, as Lazarou’s study1 shows. But human error can make the situation even worse.
Medication Errors
A survey of a 1992 national pharmacy database found a total of 429,827 medication errors from 1,081 hospitals. Medication errors occurred in 5.22% of patients admitted to these hospitals each year. The authors concluded that a minimum of 90,895 patients annually were harmed by medication errors in the country as a whole.19 A 2002 study shows that 20% of hospital medications for patients had dosage mistakes. Nearly 40% of these errors were considered potentially harmful to the patient. In a typical 300-patient hospital the number of errors per day were 40.20 Problems involving patients’ medications were even higher the following year. The error rate intercepted by pharmacists in this study was 24%, making the potential minimum number of patients harmed by prescription drugs 417,908.21
Recent Adverse Drug Reactions
More recent studies on adverse drug reactions show that the figures from 1994 (published in Lazarou’s 1998 JAMA article) may be increasing. A 2003 study followed four hundred patients after discharge from a tertiary care hospital (hospital care that requires highly specialized skills, technology, or support services). Seventy-six patients (19%) had adverse events. Adverse drug events were the most common at 66%. The next most common events were procedure-related injuries at 17%.22 In a NEJM study an alarming one in four patients suffered observable side effects from the more than 3.34 billion prescription drugs filled in 2002.23 One of the doctors who produced the study was interviewed by Reuters and commented that, “With these 10-minute appointments, it’s hard for the doctor to get into whether the symptoms are bothering the patients.”24 William Tierney, who editorialized on the NEJM study, said “… given the increasing number of powerful drugs available to care for the aging population, the problem will only get worse.” The drugs with the worst record of side effects were the SSRIs, the NSAIDs, and calcium channel blockers. Reuters also reported that prior research has suggested that nearly 5% of hospital admissions over 1 million per year are the result of drug side effects. But most of the cases are not documented as such. The study found one of the reasons for this failure: in nearly two-thirds of the cases, doctors couldn’t diagnose drug side effects or the side effects persisted because the doctor failed to heed the warning signs.
Medicating Our Feelings
We only need to look at the side effects of antidepressant drugs, which give hope to a depressed population. Patients seeking a more joyful existence and relief from worry, stress, and anxiety, fall victim to the messages blatantly displayed on TV and billboards. Often, instead of relief, they also fall victim to a myriad of iatrogenic side effects of antidepressant medication. Also, a whole generation of antidepressant users has resulted from young people growing up on Ritalin. Medicating youth and modifying their emotions must have some impact on how they learn to deal with their feelings. They learn to equate coping with drugs and not with calling on their inner resources. As adults, these medicated youth reach for alcohol, drugs, or even street drugs, to cope. According to the Journal of the American Medical Association, “Ritalin acts much like cocaine.”25 Today’s marketing of mood-modifying drugs, such as Prozac or Zoloft, makes them not only socially acceptable but almost a necessity in today’s stressful world.
Television Diagnosis
In order to reach the widest audience possible, drug companies are no longer just targeting medical doctors with their message about antidepressants. By 1995 drug companies had tripled the amount of money allotted to direct advertising of prescription drugs to consumers. The majority of the money is spent on seductive television ads. From 1996 to 2000, spending rose from $791 million to nearly $2.5 billion.26 Even though $2.5 billion may seem like a lot of money, the authors comment that it only represents 15% of the total pharmaceutical advertising budget. According to medical experts “there is no solid evidence on the appropriateness of prescribing that results from consumers requesting an advertised drug.” However, the drug companies maintain that direct to-consumer advertising is educational. Dr. Sidney M. Wolfe, of the Public Citizen Health Research Group in Washington, D.C., argues that the public is often misinformed about these ads.27 People want what they see on television and are told to go to their doctor for a prescription. Doctors in private practice either acquiesce to their patients’ demands for these drugs or spend valuable clinic time trying to talk patients out of unnecessary drugs. Dr. Wolfe remarks that one important study found that people mistakenly believe that the “FDA reviews all ads before they are released and allows only the safest and most effective drugs to be promoted directly to the public.”28
How Do We Know Drugs Are Safe?
Another aspect of scientific medicine that the public takes for granted is the testing of new drugs. Unlike the class of people that take drugs who are ill and need medication, in general, drugs are tested on individuals who are fairly healthy and not on other medications that can interfere with findings. But when they are declared “safe” and enter the drug prescription books, they are naturally going to be used by people on a variety of other medications and who also have a lot of other health problems. Then, a new phase of drug testing called Post-Approval comes into play, which is the documentation of side effects once drugs hit the market. In one very telling report, the General Accounting Office (an agency of the U.S. Government) “found that of the 198 drugs approved by the FDA between 1976 and 1985… 102 (or 51.5%) had serious post-approval risks… the serious post-approval risks (included) heart failure, myocardial infarction, anaphylaxis, respiratory depression and arrest, seizures, kidney and liver failure, severe blood disorders, birth defects and fetal toxicity, and blindness.”29 NBC’s investigative show “Dateline” wondered if your doctor is moonlighting as a drug rep. After a year-long investigation they reported that because doctors can legally prescribe any drug to any patient for any condition, drug companies heavily promote “off-label” and frequently inappropriate and non-tested uses of these medications in spite of the fact that these drugs are only approved for specific indications they have been tested for.30 The leading causes of adverse drug reactions are antibiotics (17%), cardiovascular drugs (17%), chemotherapy (15%), and analgesics and anti-inflammatory agents (15%).31
Specific Drug Iatrogenesis: Antibiotics
Dr. Egger, in a recent editorial, wrote that after fifty years of increasing use of antibiotics, 30 million pounds of antibiotics are used in America per year.32 Twentyfive million pounds of this total are used in animal husbandry. The vast majority of this amount, 23 million pounds, is used to try to prevent disease, the stress of shipping, and to promote growth. Only 2 million pounds are given for specific animal infections. Dr. Egger reminds us that low concentrations of antibiotics are measurable in many of our foods, rivers, and streams around the world. Much of this is seeping into bodies of water from animal farms. Egger says overuse of antibiotics results in food-borne infections resistant to antibiotics. Salmonella is found in 20% of ground meat but constant exposure of cattle to antibiotics has made 84% of salmonella resistant to at least one anti-salmonella antibiotic. Diseased animal food accounts for 80% of salmonellosis in humans, or 1.4 million cases per year. The conventional approach to dealing with this epidemic is to radiate food to try to kill all organisms but keep using the antibiotics that cause the original problem. Approximately 20% of chickens are contaminated with Campylobacter jejuni causing 2.4 million human cases of illness annually. Fifty-four percent of these organisms are resistant to at least one anticampylobacter antimicrobial. A ban on growth-promoting antibiotics in Denmark began in 1999, which led to a decrease from 453,200 pounds to 195,800 pounds within a year. Another report from Scandinavia found that taking away antibiotic growth promoters had no or minimal effect on food production costs. Egger further warns that in America the current crowded, unsanitary methods of animal farming support constant stress and infection, and are geared toward high antibiotic use. He says these conditions would have to be changed along with cutting back on antibiotic use. In America, over 3 million pounds of antibiotics are used every year on humans. With a population of 284 million Americans, this amount is enough to give every man, woman and child 10 teaspoons of pure antibiotics per year. Egger says that exposure to a steady stream of antibiotics has altered pathogens such as Streptococcus pneumoniae, Staplococcus aureus, and entercocci, to name a few. Almost half of patients with upper respiratory tract infections in the U.S. still receive antibiotics from their doctor.33 According to the CDC, 90% of upper respiratory infections are viral and should not be treated with antibiotics. In Germany the prevalence for systemic antibiotic use in children aged 0-6 years was 42.9%.34 Data taken from nine U.S. health plans between 1996-2000 on antibiotic use in 25,000 children found that rates of antibiotic use decreased. Antibiotic use in children, aged 3 months to under 3 years, decreased 24%, from 2.46 to 1.89 antibiotic prescriptions per/patient per/year. For children, 3 years to under 6 years, there was a 25% reduction from 1.47 to 1.09 antibiotic prescriptions per/patient per/year. And for children aged 6 to under 18 years, there was a 16% reduction from 0.85 to 0.69 antibiotic prescriptions per/ patient /per year.35 Although there was a reduction in antibiotic use, the data indicate that on average every child in America receives 1.22 antibiotic prescriptions annually. Group A beta-hemolytic streptococci is the only common cause of sore throat that requires antibiotics, penicillin and erythromycin being the only recommended treatment. However, 90% of sore throats are viral. The authors of this study estimated there were 6.7 million adult annual visits for sore throat between 1989 and 1999 in the U.S. Antibiotics were used in 73% of visits. Furthermore, patients treated with antibiotics were given non-recommended broad-spectrum antibiotics in 68% of visits. The authors noted, that from 1989 to 1999, there was a significant increase in the newer and more expensive broad-spectrum antibiotics and a decrease in use of penicillin and erythromycin, which are the recommended antibiotics.36 If antibiotics were given in 73% of visits and should have only been given in 10%, this represents 63%, or a total of 4.2 million visits for sore throat that ended in unnecessary antibiotic prescriptions between1989-1999. Dr. Richard Besser, of the CDC, in 1995, said the number of unnecessary antibiotics prescribed annually for viral infections was 20 million. Dr. Besser, in 2003, now refers to tens of millions of unnecessary antibiotics.2,2a Neither of these figures takes into account the number of unnecessary antibiotics used for non-fatal conditions such as acne, intestinal infection, skin infections, ear infections, etc.
The Problem with Antibiotics: They are Anti-Life
On September 17, 2003, the CDC relaunched a program, started in 1995, called “Get Smart: Know When Antibiotics Work.”37 This is a $1.6 million campaign to educate patients about the overuse and inappropriate use of antibiotics. Most people involved with alternative and complementary medicine have known about the dangers of overuse of antibiotics for decades. Finally the government is focusing on the problem, yet they are only putting a minuscule amount of money into an iatrogenic epidemic that is costing billions of dollars and thousands of lives. The CDC warns that 90% of upper respiratory infections, including children’s ear infections, are viral, and antibiotics don’t treat viral infection. More than 40% of about 50 million prescriptions for antibiotics each year in physicians’ offices were inappropriate.2 And using antibiotics, when not needed, can lead to the development of deadly strains of bacteria that are resistant to drugs and cause more than 88,000 deaths due to hospital-acquired infections.9 However, the CDC seems to be blaming patients for misusing antibiotics even though they are only available by prescription from a doctor who should know how to prescribe properly. Dr. Richard Besser, head of “Get Smart,” says “Programs that have just targeted physicians have not worked. Direct-to-consumer advertising of drugs is to blame in some cases.” Dr. Besser says the program “teaches patients and the general public that antibiotics are precious resources that must be used correctly if we want to have them around when we need them. Hopefully, as a result of this campaign, patients will feel more comfortable asking their doctors for the best care for their illnesses, rather than asking for antibiotics.”38 And what does the “best care” constitute? The CDC does not elaborate and patently avoids the latest research on the dozens of nutraceuticals scientifically proven to treat viral infections and boost the immune system. Will their doctors recommend vitamin C, echinacea, elderberry, vitamin A, zinc, or homeopathic oscillococcinum? No, they won’t. The archaic solutions offered by the CDC include a radio ad, “Just Say No Snort, sniffle, sneeze No antibiotics please.” Their commonsense recommendations, that most people do anyway, include resting, drinking plenty of fluids, and using a humidifier. The pharmaceutical industry claims they are all for limiting the use of antibiotics. In order to make sure that happens, the drug company Bayer is sponsoring a program called, “Operation Clean Hands”, through an organization called LIBRA.39 The CDC is also involved with trying to minimize antibiotic resistance, but nowhere in their publications is there any reference to the role of nutraceuticals in boosting the immune system nor to the thousands of journal articles that support this approach. This recalcitrant tunnel vision and refusal to use available non-drug alternatives is absolutely inappropriate when the CDC is desperately trying to curb the nightmare of overuse of antibiotics. The CDC should also be called to task for focusing only on the overuse of antibiotics. There are similar nightmares for every class of drug being prescribed today.
Drugs Pollute Our Water Supply
We have reached the point of saturation with prescription drugs. We have arrived at the point where every body of water tested contains measurable drug residues. We are inundated with drugs. The tons of antibiotics used in animal farming, which run off into the water table and surrounding bodies of water, are conferring antibiotic resistance to germs in sewage, and these germs are also found in our water supply. Flushed down our toilets are tons of drugs and drug metabolites that also find their way into our water supply. We have no idea what the long-term consequences of ingesting a mixture of drugs and drug-breakdown products will do to our health. It’s another level of iatrogenic disease that we are unable to completely measure.40-49
Specific Drug Iatrogenesis: NSAIDs
It’s not just America that is plagued with iatrogenesis. A survey of 1,072 French general practitioners (GPs) tested their basic pharmacological knowledge and practice in prescribing NSAIDs. Nonsteroidal anti-inf lammatory drugs (NSAIDs) rank first among commonly prescribed drugs for serious adverse reactions. The results of the study suggested that GPs don’t have adequate knowledge of these drugs and are unable to effectively manage adverse reactions.50 A cross-sectional survey of 125 patients attending specialty pain clinics in South London found that possible iatrogenic factors such as “over-investigation, inappropriate information, and advice given to patients as well as misdiagnosis, over-treatment, and inappropriate prescription of medication were common.” 51
Specific Drug Iatrogenesis: Cancer Chemotherapy
In 1989, a German biostatistician, Ulrich Abel, Ph.D., after publishing dozens of papers on cancer chemotherapy, wrote a monograph “Chemotherapy of Advanced Epithelial Cancer.” It was later published in a shorter form in a peer-reviewed medical journal.52 Dr. Abel presented a comprehensive analysis of clinical trials and publications representing over 3,000 articles examining the value of cytotoxic chemotherapy on advanced epithelial cancer. Epithelial cancer is the type of cancer we are most familiar with. It arises from epithelium found in the lining of body organs such as breast, prostate, lung, stomach, or bowel. From these sites cancer usually infiltrates into adjacent tissue and spreads to bone, liver, lung, or the brain. With his exhaustive review Dr. Abel concludes that there is no direct evidence that chemotherapy prolongs survival in patients with advanced carcinoma. He said that in small-cell lung cancer and perhaps ovarian cancer the therapeutic benefit is only slight. Dr. Abel goes on to say, “Many oncologists take it for granted that response to therapy prolongs survival, an opinion which is based on a fallacy and which is not supported by clinical studies.” Over a decade after Dr. Abel’s exhaustive review of chemotherapy, there seems to be no decrease in its use for advanced carcinoma. For example, when conventional chemotherapy and radiation has not worked to prevent metastases in breast cancer, high-dose chemotherapy (HDC) along with stem-cell transplant (SCT) is the treatment of choice. However, in March 2000, results from the largest multi-center randomized controlled trial conducted thus far showed that, compared to a prolonged course of monthly conventional dose chemotherapy, HDC and SCT were of no benefit.53 There was even a slightly lower survival rate for the HDC/SCT group. And the authors noted that serious adverse effects occurred more often in the HDC group than the standard-dose group. There was one treatment-related death (within 100 days of therapy) in the HDC group, but none in the conventional chemotherapy group. The women in this trial were highly selected as having the best chance to respond. There is also no all-encompassing follow-up study like Dr. Abel’s that tells us if there is any improvement in cancer-survival statistics since 1989. In fact, we need to research whether chemotherapy itself is responsible for secondary cancers instead of progression of the original disease. We continue to question why well-researched alternative cancer treatments aren’t used.
Drug Companies Fined
Periodically, a drug manufacturer is fined by the FDA when the abuses are too glaring and impossible to cover up. As one example of many, the May 2002 Washington Post reported that the maker of Claritin, Schering-Plough Corp., was to pay a $500 million fine to the FDA for quality control problems at four of its factories.54 The FDA tabulated infractions that included 90%, or 125 of the drugs they made since 1998. Besides the fine, the company had to stop manufacturing 73 drugs or suffer another $175 million dollar fine. PR statements by the company told another story. The company assured consumers that they should still feel confident in its products. Such a large settlement serves as a warning to the drug industry about maintaining strict manufacturing practices and has given the FDA more clout in dealing with drug company compliance. According to the Washington Post article, a federal appeals court ruled in 1999 that the FDA could seize the profits of companies that violate “good manufacturing practices.” Since that time Abbott Laboratories Inc. paid $100 million for failing to meet quality standards in the production of medical test kits, and Wyeth Laboratories Inc. paid $30 million in 2000 to settle accusations of poor manufacturing practices. The indictment against Schering-Plough came after the Public Citizen Health Research Group, lead by Dr. Sidney Wolfe, called for a criminal investigation of Schering-Plough, charging that the company distributed albuterol asthma inhalers even though it knew the units were missing the active ingredient.
It’s a Global Issue
A survey published in the Journal of Health Affairs pointed out that between 18% and 28% of people who were recently ill had suffered from a medical or drug error in the previous two years. The study surveyed 750 recently-ill adults in five different countries. The breakdown by country showed 18% of those in Britain, 25% in Canada, 23% in Australia, 23% in New Zealand, and the highest number was in the U.S. at 28%.55
Warehousing Our Elders
The fact that there are very few statistics on malnutrition in acute-care hospitals and nursing homes shows the lack of concern in this area. A survey of the literature turns up very few American studies. Those that do appear are foreign studies in Italy, Spain, and Brazil. However, there is one very revealing American study conducted over a 14-month period that evaluated 837 patients in a 100-bed sub-acute care hospital for their nutritional status. Only 8% of the patients were found to be well nourished. Almost one-third (29%) were malnourished and almost two-thirds (63%) were at risk of malnutrition. The consequences of this state of deficiency were that 25% of the malnourished patients required readmission to an acute-care hospital compared to 11% of the well-nourished patients. The authors concluded that malnutrition reached epidemic proportions in patients admitted to this sub-acute-care facility.56 Many studies conclude that physical restraints are an under-reported and preventable cause of death. Whereas administrators say they must use restraints to prevent falls, in fact, they cause more injury and death because people naturally fight against such imprisonment. Studies show that compared to no restraints, the use of restraints carries a higher mortality rate and economic burden.57-59 Studies found that physical restraints, including bedrails, are the cause of at least 1 in every 1,000 nursing-home deaths.60-62 However, deaths caused by malnutrition, dehydration, and physical restraints are rarely recorded on death certificates. Several studies reveal that nearly half of the listed causes of death on death certificates for older persons with chronic or multi-system disease are inaccurate.63 Even though 1-in-5 people die in nursing homes, the autopsy rate is only 0.8%.64 Thus, we have no way of knowing the true causes of death.
Over-Medicating Seniors
Dr. Robert Epstein, chief medical officer of Medco Health Solutions Inc. (a unit of Merck & Co.), conducted a study on drug trends.65 He found that seniors are going to multiple physicians and getting multiple prescriptions and using multiple pharmacies. Medco oversees drug benefit plans for more than 60 million Americans, including 6.3 million senior citizens who received more than 160 million prescriptions. According to the study the average senior receives 25 prescriptions annually. In those 6.3 million seniors a total of 7.9 million medication alerts were triggered: less than half that number, 3.4 million, were detected in 1999. About 2.2 million of those alerts indicated excessive dosages unsuitable for senior citizens and about 2.4 million indicated clinically inappropriate drugs for the elderly. Reuters interviewed Kasey Thompson, director of the Center on Patient Safety at the American Society of Health System Pharmacists, who said, “There are serious and systemic problems with poor continuity of care in the United States.” He says this study shows “the tip of the iceberg” of a national problem. According to Drug Benefit Trends, the average number of prescriptions dispensed per non-Medicare HMO member per year rose 5.6% from 1999 to 2000 from 7.1 to 7.5 prescriptions. The average number dispensed for Medicare members increased 5.5% from 18.1 to 19.1 prescriptions.66 The number of prescriptions in 2000 was 2.98 billion, with an average per person prescription amount of 10.4 annually.66 In a study of 818 residents of residential care facilities for the elderly, 94% were receiving at least one medication at the time of the interview. The average intake of medications was five per resident; the authors noted that many of these drugs were given without a documented diagnosis justifying their use.67
What Remains To Be Uncovered
Iatrogenic morbidity, mortality, and financial loss in outpatient clinics, transitional care, long-term care, rehabilitative care, home care, private practitioners offices, as well as hospitals, is also due to the following:
- X-ray exposures: mammography, fluoroscopy, CT scans.
- Overuse of antibiotics in all conditions.
- Drugs that are carcinogenic: hormone replacement therapy
- Immunosuppressive drugs, prescription drugs.
- Cancer chemotherapy: If it doesn’t extend life, is it shortening life?
- Surgery and surgical procedures.
- Unnecessary surgery: Cesarean section, radical mastectomy, preventive mastectomy, radical hysterectomy, prostatectomy, cholecystectomies, cosmetic surgery, arthroscopy.
- Medical procedures and therapies.
- Discredited, unnecessary, and unproven medical procedures and therapies.
- Doctors themselves: when doctors go on strike, it appears the mortality rate goes down.
- Missed diagnoses.
Conclusion
What we have outlined in this paper are insupportable aspects of our contemporary medical system that need to be changed, beginning at its very foundations. When the number one killer in a society is the healthcare system, that system must take responsibility for its shortcomings. It’s a failed system in need of immediate attention.
References
- Lazarou J, Pomeranz B, Corey P: Incidence of adverse drug reactions in hospitalized patients. JAMA, 1998; 279:1200-1205.
- Rabin R: Caution About Overuse of Antibiotics. Newsday, Sept. 18, 2003
2a. http://www.cdc.gov/drugresistance/community - Calculations detailed in Unnecessary Surgical Procedures section, from two sources: (13) http://hcup.ahrq.gov/HCUPnet.asp (see Instant Tables: 2001 prerun tables: most common procedures) and (71) US Congressional House Subcommittee Oversight Investigation. Cost and Quality of Health Care: Unnecessary Surgery. Washington, DC: Government Printing Office, 1976.
- Calculations from four sources, see Unnecessary Hospitalization section: (13) http:// hcup.ahrq.gov/HCUPnet.asp (see Instant Tables: 2001 prerun tables: most common diagnoses) and (93) Siu AL, Sonnenberg FA, Manning WG, et al: Inappropriate use of hospitals in a randomized trial of health insurance plans.
NEJM, 1986; Nov 13/315(20):1259-66. and (94) Siu AL, Manning WG, Benjamin B. Patient, provider and hospital characteristics associated with inappropriate hospitalization. Am J Public Health, 1990; Oct/80(10):1253-6. and (95) Eriksen BO, Kristiansen IS, Nord E, Pape JF, Almdahl SM, Hensrud A, Jaeger S. The cost of inappropriate admissions: a study of health benefits and resource utilization in a department of internal medicine. J Intern Med, 1999; Oct/246(4):379-87. - National Vital Statistics Reports. Vol. 51, No. 5, March 14, 2003.
- Thomas et al., 2000; Thomas et al., 1999. Institute of Medicine.
- Xakellis GC, Frantz R, Lewis A: Cost of Pressure Ulcer Prevention in Long Term Care, JAGS, 43-5, May 1995.)
- Barczak CA, Barnett RI, Childs EJ, Bosley LM: “Fourth National Pressure Ulcer Prevalence Survey,” Advances in Wound Care, 1997; Jul/Aug: 10- 4.
- Weinstein RA: Nosocomial Infection Update. Special Issue. Emerging Infectious Diseases. 1998; July/Sept: Vol 4, No. 3.
- Fourth Decennial International Conference on Nosocomial and Healthcare-Associated Infections, Morbidity and Mortality Weekly Report (MMWR), 2000, Feb. 25, Vol. 49, No. 7: 138.
- Greene Burger S, Kayser-Jones J, Prince Bell J: Malnutrition and Dehydration in Nursing Homes: Key Issues in Prevention and Treatment. National Citizens’ Coalition for Nursing Home Reform. June 2000. http://www.cmwf.org/ programs/elders/burger_mal_386.asp
- Starfield B: Is US health really the best in the world? JAMA. 2000 Jul 26;284(4):483-5. Starfield B. Deficiencies in US medical care. JAMA, 2000; Nov 1, 284(17): 2184-5.
- HCUPnet, Healthcare Cost and Utilization Project for the Agency for Healthcare Research and Quality. http://www.ahrq.gov/data/hcup/hcupnet.htm, http://hcup.ahrq.gov/HCUPnet.asp, http://hcup.ahrq.gov/HCUPnet.asp
- Leape L: National Patient Safety Foundation Press Release. Nationwide Poll on Patient Safety Oct 9, 1997 New York. http://www.npsf.org/ html/pressrel/finalgen.html
- Leape LL: Error in medicine. JAMA, 1994; Dec 21, 272(23): 1851-7.
15a. Brennan TA, Leape LL, Laird NM, et al: Incidence of adverse events and negligence in hospitalized patients. N Engl J Med, 1991; 324: 370-376. - Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group. JAMA, 1995; Jul 5, 274(1): 29-34.
- Vincent C, Stanhope N, Crowley-Murphy M: Reasons for not reporting adverse incidents: an empirical study. J Eval Clin Pract, 1999 Feb; 5(1): 13-21.
- Wald H, Shojania K: Incident Reporting in Making Health Care Safer: A Critical Analysis of Patient Safety Practices, Agency for Healthcare Research and Quality (AHRQ), 2001.
- Bond CA, Raehl CL, Franke T: Clinical pharmacy services, hospital pharmacy staffing, and medication errors in United States hospitals.
Pharmacotherapy, 2002; Feb 22(2):134-47. - Barker KN, Flynn EA, Pepper GA, et al: Medication errors observed in 36 health care facilities. Arch Intern Med, 2002; Sep 9, 162(16):1897- 903.
- LaPointe NM, Jollis JG: Medication errors in hospitalized cardiovascular patients. Arch Intern Med, 2003; Jun 23, 163(12): 1461-6.
- Forster AJ, Murff HJ, Peterson JF, et al: The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med, 2003; Feb 4, 138(3): 161-7.
- Gandhi TK, Weingart SN, Borus J, et al: Adverse drug events in ambulatory care. N Engl J Med, 2003; Apr 17, 348(16): 1556-64.
- Medication side effects strike 1-in-4. Reuters. April 17, 2003
- Vastag B: Pay attention: ritalin acts much like cocaine. JAMA, 2001 Aug 22-29;286(8):905-6.
- Rosenthal MB, Berndt ER, Donohue JM, Frank RG, Epstein AM: Promotion of prescription drugs to consumers. N Engl J Med, 2002; Feb 14, 346(7): 498-505.
- Wolfe SM: Direct-to-consumer advertising—education or emotion promotion? N Engl J Med, 2002; Feb 14, 346(7): 524-6.
- Ibid.
- GAO/PEMD 90-15 FDA DRUG Review: Post-approval Risks, 1976-1985; 3.
- MSNBC, July 11, 2003
- Suh DC, Woodall BS, Shin SK, Hermes-De Santis ER: Clinical and economic impact of adverse drug reactions in hospitalized patients. Ann Pharmacother, 2000; Dec 34, (12): 1373-9.
- Egger WA: Antibiotic Resistance: Unnatural Selection in the Office and on the Farm. Wisconson Medical Journal, Aug. 2002.
- Nash DR, Harman J, Wald ER, Kelleher KJ: Antibiotic prescribing by primary care physicians for children with upper respiratory tract infections. Arch Pediatr Adolesc Med, 2002 Nov; 156(11): 1114-9.
- Schindler C, Krappweis J, Morgenstern I, Kirch W. Pharmacoepidemiol Drug Saf. 2003; Mar; 12(2): 113-20.
- Finkelstein JA, Stille C, Nordin J, et al: Reduction in antibiotic use among US children, 1996- 2000. Pediatrics, 2003; Sep. 11, 2(3 Pt 1): 620-7.
- Linder JA, Stafford RS: Antibiotic treatment of adults with sore throat by community primary care physicians: a national survey, 1989-1999.
JAMA, 2001; Sep 12, 286(10): 1181-6. - http://www.cdc.gov/drugresistance/community
- http://www.health.state.ok.us/program/cdd/ar
- http://www.librainitiative.com/en/ap/or/ li_ap_or_op.html
- Ohlsen K, Ternes T, Werner G, et al: Impact of antibiotics on conjugational resistance gene transfer in Staphylococcus aureus in sewage. Environ Microbiol, 2003; Aug, 5(8): 711-6.
- Pawlowski S, Ternes T, Bonerz M, et al: Combined in situ and in vitro assessment of the estrogenic activity of sewage and surface water samples. Toxicol Sci, 2003; Sep, 75(1): 57-65. Epub 2003 Jun 12.
- Ternes TA, Stuber J, Herrmann N, et al: a tool for removal of pharmaceuticals, contrast media and musk fragrances from wastewater? Water Res. 2003; Apr 37(8):1976-82.
- Ternes TA, Meisenheimer M, McDowell D, et al: Removal of pharmaceuticals during drinking water treatment. Environ Sci Technol, 2002; Sep 1, 36(17):3855-63.
- Ternes T, Bonerz M, Schmidt T. Determination of neutral pharmaceuticals in wastewater and rivers by liquid chromatography-electrospray tandem mass spectrometry. J Chromatogr A, 2001; Dec 14, 938(1-2): 175-85.
- Golet EM, Alder AC, Hartmann A, et al: Trace determination of fluoroquinolone antibacterial agents in urban wastewater by solid-phase extraction and liquid chromatography with fluorescence detection. Analyt Chem, 2001; Aug 1, 73(15): 3632-8.
- Daughton CG, Ternes TA. Pharmaceuticals and personal care products in the environment: agents of subtle change? Environ Health Perspect, 1999; Dec, 107 Suppl 6: 907-38. Review.
- Hirsch R, Ternes T, Haberer K, Kratz KL. Occurrence of antibiotics in the aquatic environment. Sci Total Environ, 1999; Jan 12, 225 (1-2): 109-18.
- Ternes TA, Stumpf M, Mueller J, et al: Behavior and occurrence of estrogens in municipal sewage treatment plants I. Investigations in Germany, Canada and Brazil. Sci Total Environ, 1999; Jan 12, 225(1-2): 81-90.
- Hirsch R, Ternes TA, Haberer K, et al: Determination of antibiotics in different water compartments via liquid chromatographyelectrospray tandem mass spectrometry. J Chromatogr A, 1998; Jul 31, 815(2): 213-23.
- Coste J, Hanotin C, Leutenegger E. Prescription of non-steroidal anti-inflammatory agents and risk of iatrogenic adverse effects: a survey of 1072 French general practitioners. Therapie, 1995; May-Jun, 50(3): 265-70.
- Kouyanou K, Pither CE, Wessely S. Iatrogenic factors and chronic pain. Psychosom Med, 1997; Nov-Dec, 59(6): 597-604.
- Abel U: Chemotherapy of advanced epithelial cancer—a critical review. Biomed Pharmacother, 1992; 46(10): 439-52.
- Schulman KA, Stadtmauer EA, Reed SD, et al: Economic analysis of conventional-dose chemotherapy compared with high-dose chemotherapy plus autologous hematopoietic stem-cell transplantation for metastatic breast cancer. Bone Marrow Transplant, 2003; Feb 31(3): 205-10.
- Kaufman M: Washington Post, May 18, 2002; Page A01.
- Five Nation Survey Exposes Flaws in the U.S. Health Care System. May 14, 2002. Journal of Health Affairs.
- Thomas DR, et al: Malnutrition in subacute care. Am J Clin Nutr, 2002; Feb, 75(2): 308-13.
- Robinson BE. Death by destruction of will. Lest we forget. Arch Intern Med, 1995; Nov 13, 155(20): 2250-1.
- Capezuti E. et al. The relationship between physical restraint removal and falls and injuries among nursing home residents. J Gerontol Biol Sci Med Sci, 1998; Jan, 53(1): M47-52.
- Phillips CD, Hawes C, Fries BE: Reducing the use of physical restraints in nursing homes: will it increase costs? Am J Public Health, 1993; Mar, 83(3): 342-8.
- Miles SH, Irvine P: Deaths caused by physical restraints. Gerontologist, 1992; Dec, 32(6): 762-6.
- Annas GJ: The Last Resort–The Use of Physical Restraints in Medical Emergencies. N Engl J Med, 1999; Oct 28, 341(18):1408-12.62. Parker K. et al. Deaths caused by bedrails. J Am Geriatr Soc, 45(7):797-802 1997 Jul.
- Miles SH: Concealing accidental nursing home deaths. HEC Forum, 2002; Sep 14(3): 224-34.
- Lloyd-Jones DM, Martin DO, Larson MG, Levy D: Accuracy of death certificates for coding coronary heart disease as the cause of death. Ann Intern Med, 1998; Dec 15, 129(12):1020-6.
- Katz PR, Seidel G: Nursing home autopsies. Survey of physician attitudes and practice patterns. Arch Pathol Lab Med, 1990; Feb, 114(2): 145-7.
- Bordon W: “Study Finds Overmedication of U.S. Seniors. Reuters Health, May 21, 2003.
- Average Number of Prescriptions by HMOs Increases. Drug Benefit Trends, 2002; 12/9,Vol 14, No 8.
- Prescription Drug Trends, 2001; Nov, Kaiser Family Foundation.
- Berens D: Unhealthy Hospitals: Infection epidemic carves deadly path. Poor hygiene, overwhelmed workers contribute to thousands of deaths. The Chicago Tribune, 2002; July 21, http://www.chicagotribune.com/news/specials/ chi-0207210272jul21.story
- http://www.imakenews.com/health-itworld/ e_article000187752.cfm
- Weingart SN, McL Wilson R, Gibberd RW, Harrison B: Epidemiology of medical error. West J Med, 2000; Jun, 172(6): 390-3.
- Zhan C, Miller M: Excess Length of Stay, Charges, and Mortality Attributable to Medical Injuries During Hospitalization. AHRQ Study. JAMA, 2003; 290: 1868-1874.